
Prenatally, severe types may be difficult to distinguish from thanatophoric dysplasia (missense mutations in fibroblast growth factor receptor3), campomelic dysplasia (mutations in or near the SOX9 gene), and achondrogenesis type I (type 1A etiology is unknown, type 1B is caused by mutations in the SLC26A2 gene). A positive family history is usually not present, because appearance of classical OI in children of unaffected parents is caused by parental mosaicism. About 5 % of OI cases are not caused by defects in either, type I collagen or the P3H1 complex.īecause the types of OI vary widely in symptoms, clinical appearance and in their onset, the diagnosis varies with the age of the individuals. Autosomal recessive OI is caused by defects in proteins of the prolyl3hydroxylation (P3H1) complex, CRTAP, LEPRE1 and PPIB or helical folding (FKBP10, SERPINH1). In types II, III and IV a mixture of normal collagen and collagen with a structural defect is synthesized.ĭevelopments in recent years have shown the genetic background of relatively rare recessive OI. The moderate and severe types of autosomal dominant OI are caused by structural defects in one of the two chains encoding for the type I collagen heterotrimer. Individuals with type I OI synthesize a reduced amount of structurally normal type I collagen because of a null COL1A1 allele, with a relative increase in the COL2/COL1 ratio.

Consecutively molecularbiological studies have shown that the mild Sillence type I OI is caused by quantitiative defects in type I collagen. He divided OI into four subtypes, based on clinical and radiographic features. Classical OI has been described by Sillence in 1979.
OSTEOGENESIS IMPERFECTA TYPE 3 SKIN
Аbout 85–90 % of patients with clinical OI have abnormalities of type I collagen, the major structural component of the extracellular matrix of bone, skin and tendon, caused by an autosomal dominant pattern.
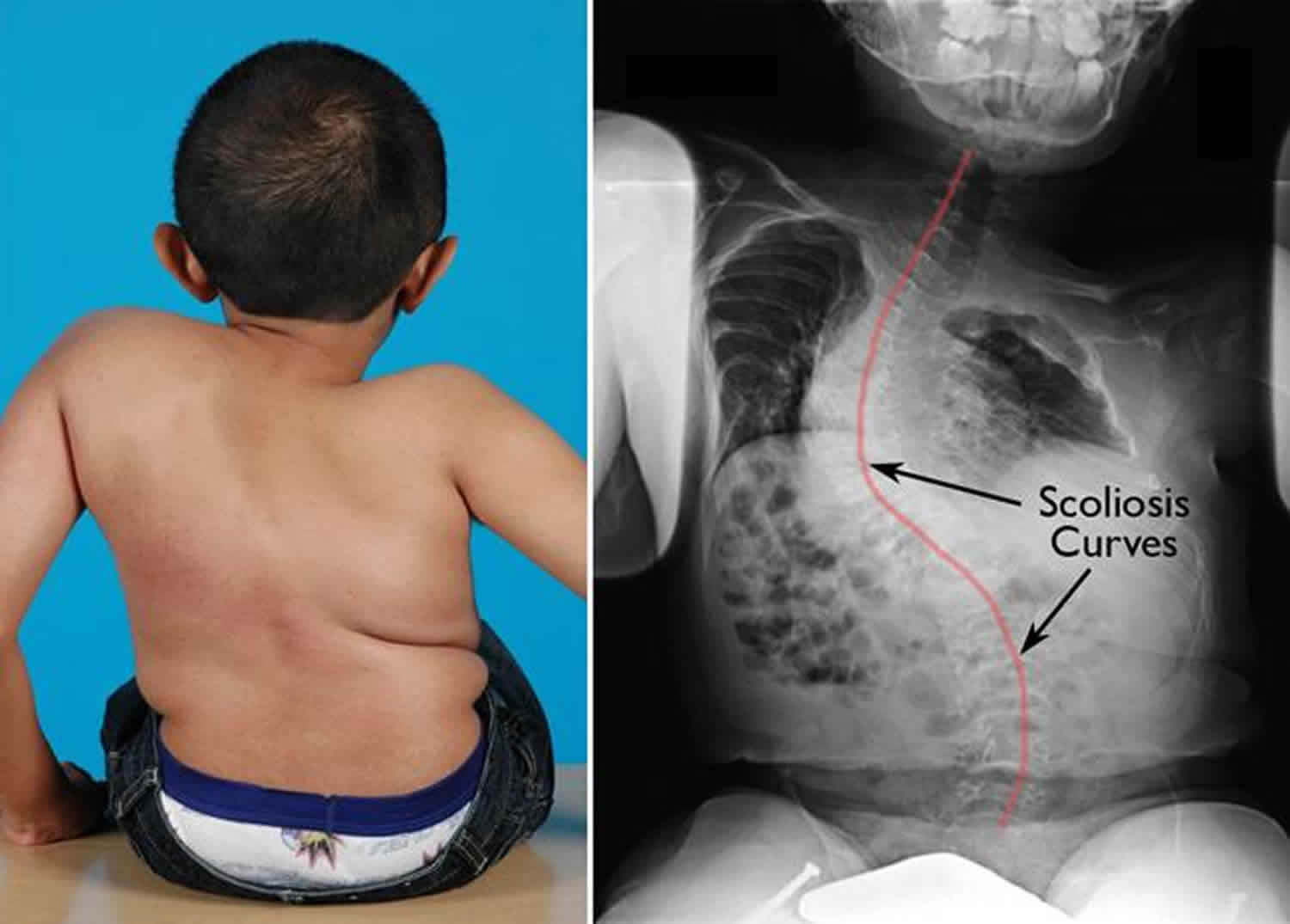
Patients with OI may have growth deficiency, wormian bones, scoliosis and extraskelatal manifestations such as defective tooth formation (dentinogenesis imperfecta), hearing loss, macrocephaly, blue sclerae, barrel chest up to hyperlaxity of joints and ligaments. The clinical range of this condition is extremely broad, ranging from lethal cases in the perinatal period to cases that may be difficult to detect in later life and can pretend early osteoporosis. Osteogenesis imperfecta (OI), also known as brittle bone disease, is a genetic disorder of connective tissue characterized by fragile bones and a susceptibility to fracture from mild trauma.


 0 kommentar(er)
0 kommentar(er)
